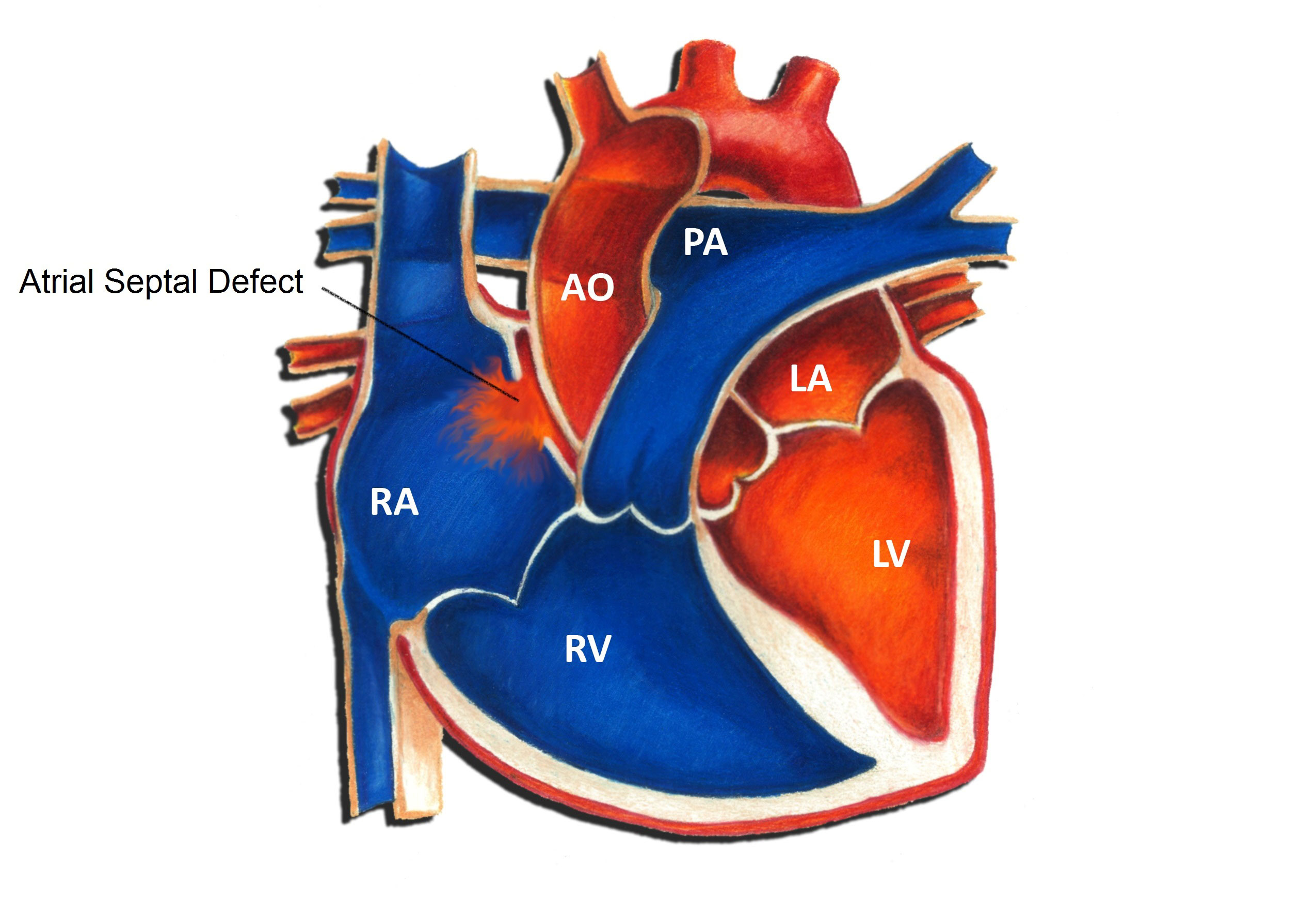
An atrial septal defect (ASD) is a hole in the atrial septum, the upper wall of the heart separating the right and left atria. Intervention is occasionally necessary to close an ASD. This most commonly occurs in the setting of a large or moderate size defect. The most common indication for intervention is the presence of dilation of heart chambers, specifically the right ventricle, due to long-standing excess blood flow. Typically intervention is performed between 2 and 5 years of age, although it can easily be accomplished earlier if necessary.
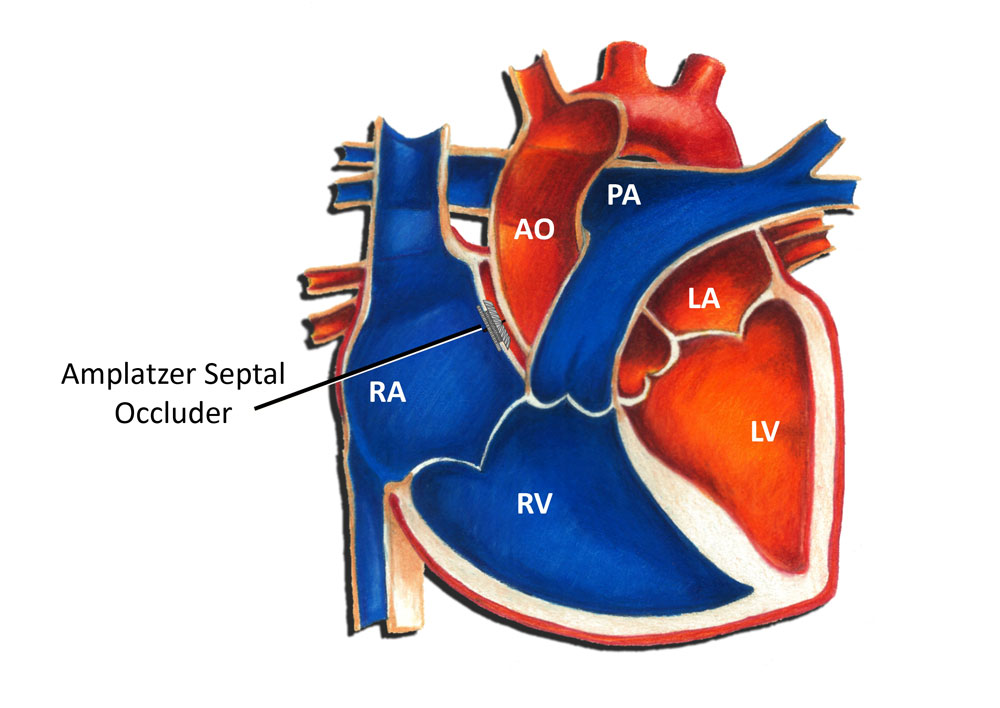
The first successful surgery to close an ASD was performed in 1952 by John Lewis and associates at the University of Minnesota. Starting in the 1970s, physicians began experimenting with the idea of closing ASD's through a less invasive procedure. Device closure of an atrial septal defect via a cardiac catheterization was first successfully performed in 1975 by King and Mills at the Ochsner Clinic in New Orleans. The most commonly used device today is the Amplatzer septal occluder, developed in the 1990s by Dr. Kurt Amplatz. The Amplatzer septal occluder is a self-centering device with two circular retaining discs that are made of a nitinol wire mesh connected by a short connecting waist. The waist centers the device, as well as occludes the defect.
The device is placed via a cardiac catheterization. A catheter (a long thin flexible tube), is placed into the heart through a blood vessel in the leg. Once the device position is confirmed, the device is released and effectively closes the ASD from the inside. Once the device is adequately positioned, there is little to no risk of it coming free. The vast majority of patients who undergo device closure of an ASD spend one night in the hospital and are discharged home the following day. They are usually back to full activity within the week.
The long-term prognosis for a patient undergoing ASD closure either by surgery or device closure is outstanding. The vast majority of patients have no significant problems whatsoever long-term.
All patients who undergo either surgery or device closure of an ASD are required to take antibiotics before any dental or surgical procedures for at least 6 months following the procedure. This precaution is designed to minimize the risk of any bacterial infection forming in the heart tissue. This can happen with dental work and certain forms of surgery. After 6 months, usually the normal heart tissue has sealed things in place sufficiently to no longer require this.

