Coarctation of the Aorta
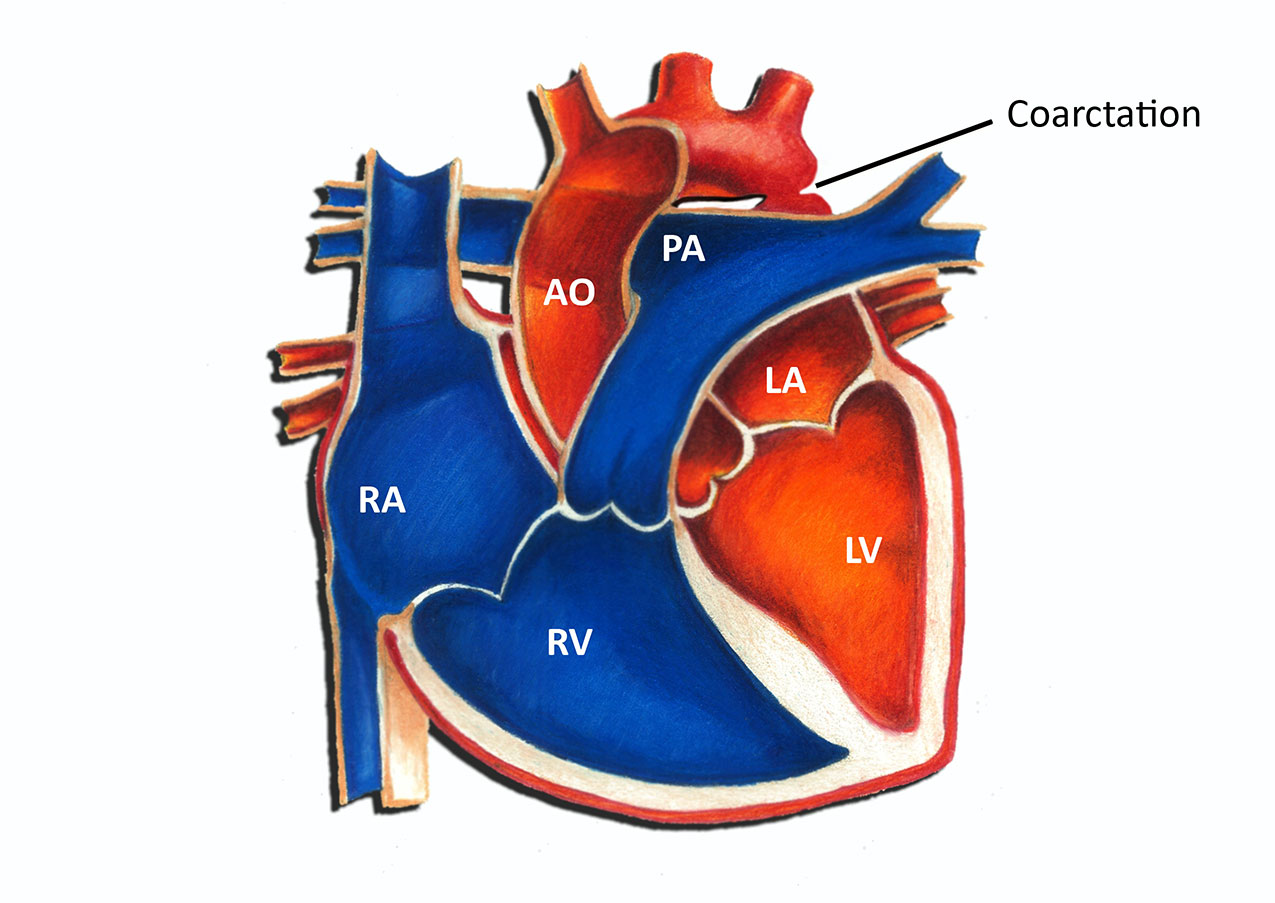
Coarctation of the aorta is a narrowing of the aorta, the main blood vessel carrying oxygen-rich blood from the left ventricle of the heart to all of the organs of the body. Coarctation occurs most commonly in a short segment of the aorta adjacent to the ductus arteriosus.
The ductus arteriosus is a blood vessel normally present in all fetuses that forms a connection between the pulmonary artery and the aorta. The ductus arteriosus has special oxygen-sensing tissue in its wall that causes it to close in the first hours or days of life. It is thought that coarctation may be caused by the presence of extra ductal tissue extending into the adjacent aorta which results in aortic narrowing as the ductal tissue contracts.
Incidence and Associated conditions
Congenital heart defects occur in 1:100 pregnancies, and coarctation represents approximately 5% of these defects. Coarctation may occur in isolation or in association with other heart defects involving the left side of the heart, such as a bicuspid aortic valve or ventricular septal defect. Coarctation may also be seen as a part of more complex defects, such as hypoplastic left heart syndrome. Coarctation of the aorta is common in patients with some chromosomal abnormalities, such as Turner's syndrome.
Symptoms of Coarctation
The symptoms and age at presentation of coarctation depend on the severity of the narrowing. In approximately 50 percent of cases of isolated coarctation, the narrowing is severe enough to cause symptoms in the first days of life when the ductus arteriosus closes. When the ductus arteriosus closes, the left ventricle must suddenly pump against much higher resistance which can lead to symptoms of heart failure or shock, such as respiratory distress or lethargy. Because these newborns are well up until the ductus arteriosus closes, symptoms appear rapidly and are often severe.
In mild cases of coarctation, symptoms may be subtle and the diagnosis may not be made for several years. After infancy, the most frequent findings leading to the detection of coarctation are a heart murmur, diminished lower extremity pulses, or hypertension in the arms.
Diagnosis
The diagnosis of coarctation is usually made with an echocardiogram, which can define the anatomy of the aorta and evaluate for other cardiac anomalies. Occasionally in older children the region of coarctation is difficult to image well by echocardiography. In such cases, MRI or CT scan may be used. Cardiac catheterization is occasionally necessary for diagnosis.
Management and Treatment
In a critically ill newborn, a continuous intravenous medication, prostaglandin (PGE-1), is used to open the ductus arteriosus allowing blood to flow to areas beyond the coarctation. Once the patient is stabilized, there are a number of surgical techniques to repair coarctation. The severity and length of the coarctation segment will dictate the most appropriate technique. Most commonly surgery involves removing the narrowed segment and reattaching the ends in what is called an end to end anastomosis, as shown in the diagram below. More information on this procedure can be found in the article titled Coarctation of the Aorta - Surgical Repair.
